One stormy November night in 2016, a horror story unfolded across Melbourne.
Amidst strong winds and hail, thousands of people simultaneously started struggling to breathe.
There was a 681% increase in asthma-related hospital admissions, and 10 people died. Some of them had never experienced asthma symptoms prior to the storm.
This event is the most severe recorded case of a phenomenon known as epidemic thunderstorm asthma.
But how does one thunderstorm trigger thousands of asthma attacks? And how are we monitoring the risk of future events?
IT’S NOT EASY BEING WHEEZY
To understand epidemic thunderstorm asthma, we need to understand asthma itself.
Asthma is a chronic non-communicable disease affecting around 1 in 9 Australians.
People with asthma experience coughing, wheezing and shortness of breath due to inflammation and narrowing of small airways in their lungs.
Asthma symptoms can be worsened by a variety of triggers, including illness, allergens like pollen and fur and changes in the weather.
A sudden onset of symptoms is called an asthma attack, and it can be life threatening.
Fortunately, for people with access to healthcare, asthma is easily treatable. Currently, most asthma medications are delivered directly to the lungs through an inhaler.
However, if you’ve never experienced asthma before, it’s unlikely that you’ll have the correct medication on hand. And that’s what makes epidemic thunderstorm asthma events so dangerous.
A PERFECT STORM
The cause of epidemic thunderstorm asthma is not fully understood. And it seems that it can’t happen everywhere.
So far, within Australia, Victoria and New South Wales are considered to be at risk of experiencing epidemic thunderstorm asthma. However, there’s no indication that it could happen in Western Australia.
When the event does happen, from what research has found so far, it seems to require an unlucky combination of environmental factors.
First, the level of airborne grass pollen has to be high. This is usually when grasses are flowering. In Melbourne, this is from November to late December each year. During this period, people with hay fever will already be experiencing discomfort.
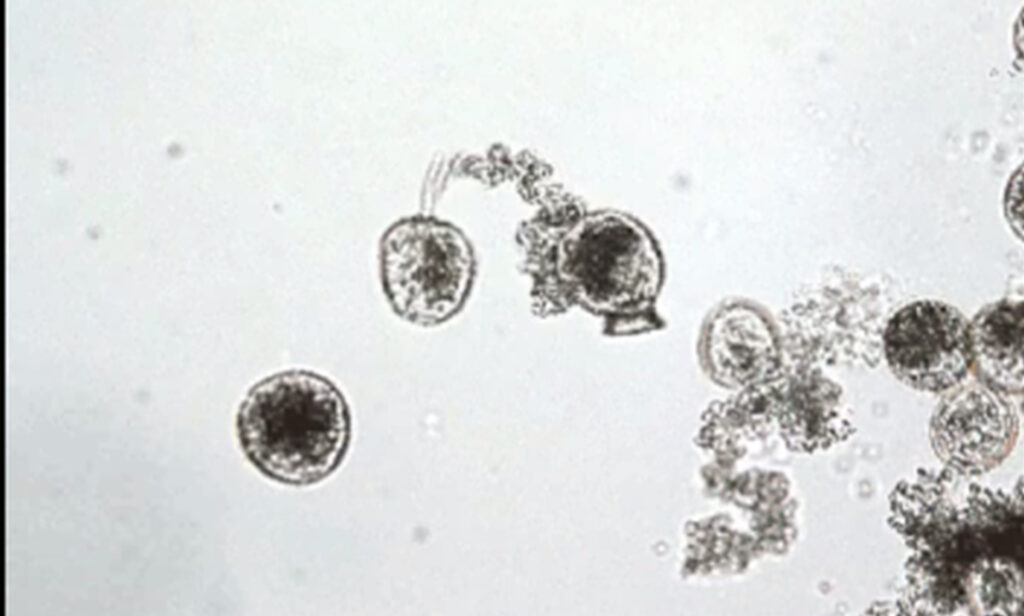
Second, there has to be a storm. The rain or humidity from a thunderstorm can cause individual granules of pollen to burst apart, flinging hundreds to thousands of minuscule allergy-causing particles into the air. These tiny pieces can then be picked up by strong winds and dispersed over large areas.
Usually, our nose and upper airways can filter out larger pollen particles. But these smaller particles bypass our defences and travel deep into the lungs, causing an allergic response and potentially an asthma attack.
And that’s essentially how the rare epidemic thunderstorm asthma occurs.
SCIENCE IN A- AA- ACTION
After the 2016 thunderstorm asthma incident, the Victorian Government launched a strategy to be better prepared for next time. This included spreading awareness, reviewing the emergency response system and building a world-class forecasting system.
The system was developed in collaboration with organisations including the CSIRO, Bureau of Meteorology (BOM), University of Melbourne and Deakin University. It uses statistical computer modelling to predict the risk of thunderstorm asthma 3 days into the future.
To do this, the system needs to calculate the likelihood of grass pollen and the weather creating a deadly combination.
It’s a complex model requiring data from a number of sources like pollen-monitoring stations, satellite observations of grassy areas and weather data from BOM.
Through proper analysis, all of this data allows us to forecast the likelihood of a thunderstorm asthma incident occurring. This helps vulnerable people make decisions like staying indoors or carrying an inhaler.
CHANGING CONDITIONS AHEAD
The Victorian forecasting system has been active since 2017, providing health information for Melbourne and surrounding areas.
However, climate change is contributing to shifting distributions of grasses and increasing the amount of grass pollen in the air. This means thunderstorm asthma events could start occurring in new areas of southeastern Australia, with at-risk areas expanding outwards from the locations of past events.
As environmental conditions change, epidemic thunderstorm asthma events may become common. And as a key component of our emergency public health response, developments in our cutting-edge forecasting system will become increasingly important in keeping us safe.