Viruses are an inescapable part of human existence—from the mild inconvenience of the common cold to society-crushing pandemics. Viruses’ ability to evolve and adapt to overcome our best defences makes them dangerous foes to humanity. When a particularly deadly virus grows in a world region without access to high-quality healthcare, the results can be disastrous.
Ameh James, a PhD researcher in molecular biology from USC, is fighting the resurgence of one of the most deadly viruses in recent years, Ebola. To do this, he has developed a test that can detect the earliest stages of Ebola virus in just 30 minutes.
“It started in 2015 when I first arrived in Australia on my PhD scholarship. I remember coming home after a day’s work in the lab. I turned on the news, and Ebola virus was killing a lot of people in Africa. It was spreading to other countries. Everybody was scared,” Ameh says.
“I asked myself how I could contribute. That’s when I thought of developing a simple Ebola test.”
BREAKING DOWN EBOLA TESTS
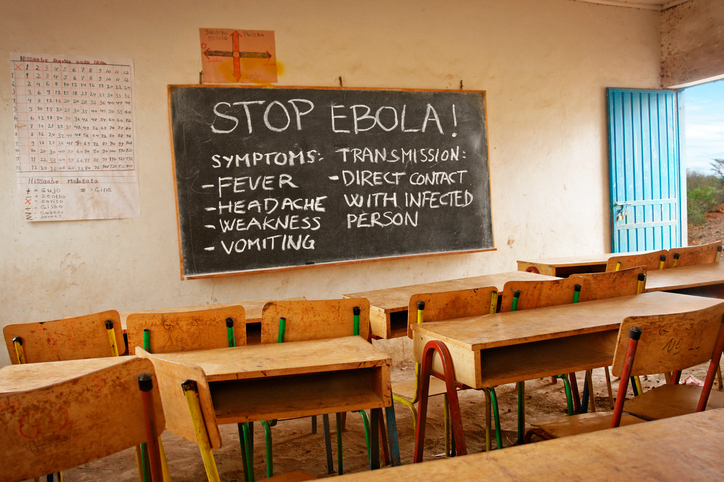
A common way to test for viruses is to look for antigens.
Antigens are proteins on the surface of a viral cell that our antibodies use to find and kill the virus. Basically, the antigen is the target for the immune system to seek and destroy. It’s also the target for many of our current Ebola tests.
But early detection is a problem in antigen tests. Most tests work by changing colour in the presence of Ebola antigens reacting with our antibodies. However, if the virus hasn’t spread enough within a person, the reaction won’t be big enough for the detector.

“In the traditional Ebola test, the body would need to develop a certain number of antibodies before the test worked. My test isn’t looking for these antigens so we don’t have to wait for antibodies to develop. This helps us detect the virus earlier,”
BEATING THE SYSTEM
Another problem is a virus’s antigens change form as it evolves. This allows Ebola to hide from our antibodies and our tests. Viruses can evolve very quickly, so virus tests that use these antigen markers must be constantly updated.
Ameh wanted to create an Ebola test that would continue to find new strains of Ebola as the virus evolved.
To do this, Ameh tested the Ebola virus’s ribonucleic acid strand (RNA). RNA takes a similar role in viruses to its bigger brother, DNA. Ebola’s RNA strand carries the virus’s genetic blueprint and infects our cells with it, turning them into factories for making more Ebola.
RNA testing catches Ebola earlier because the RNA collected from blood is amplified in a test tube for 30 minutes before testing. Because of this growth period, Ameh’s test can detect Ebola at earlier stages than antigen detection tests such as ReEBOV and OraQuick.
By targeting Ebola’s RNA strand, the test is future-proofed against new strains with different antigens. It also allows the disease to be detected much earlier. Ebola can kill over half those infected, so catching it early is critical to stopping the spread.
THE SURVIVABILITY TEST
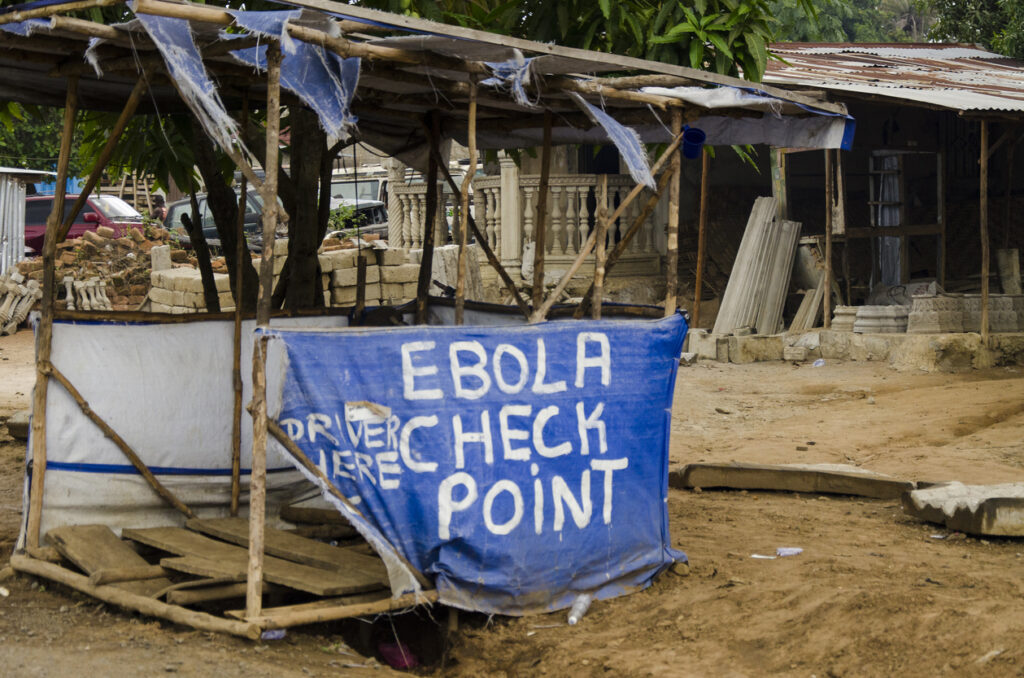
It’s not just about early detection. In many of the poorest areas of West Africa, medical services are limited. Ameh’s test is cheap, easy to use and requires only basic medical equipment. This makes it a powerful tool for combating Ebola in poverty-stricken areas.
“I worked in Africa for more than 10 years as a pathologist. Our labs don’t have the resources we have here. There are issues with power and water supply, but also space. It’s very difficult to have testing equipment and keep it running,” Ameh says.
“Also, not many people are trained in lab practices. Sample contamination is a big problem. To stop this, I made my test easy. All you need to do is stick the sample into my testing kit and put it straight into a machine most labs already have.”
The Ebola epidemic scared the world when discovered, but in places like Liberia and Guinea, it tore apart entire communities. Despite this tragedy, we’re learning more about viral outbreaks and creating better defences for the future. With tests like those created by Ameh James, we’re fighting back and saving lives.