A recent study led by Curtin University has found it’s possible to predict the chances of an individual developing liver cancer by using RNA sequencing.
Over 2000 Australians are diagnosed with primary liver cancer each year.
“75% of these people are already in the intermediary or advanced stage of cancer when they are diagnosed,” says Dr Rodrigo Carlessi, the lead author of the new study.
“Palliative treatment is often the only option.”
How liver cancer is currently diagnosed | Cancer Council NSW
With any type of cancer, early detection is key to survival. Rodrigo and his team at the Curtin Health Innovation Research Institute wanted to know if there was a way to predict the development of liver cancer.
“What is unique about our research is that we are predicting the risk of developing liver cancer rather than just early detection of cancer,” says Rodrigo.
Once identified, at-risk people could reduce their chances of developing liver cancer through lifestyle changes.
Technological advancement key
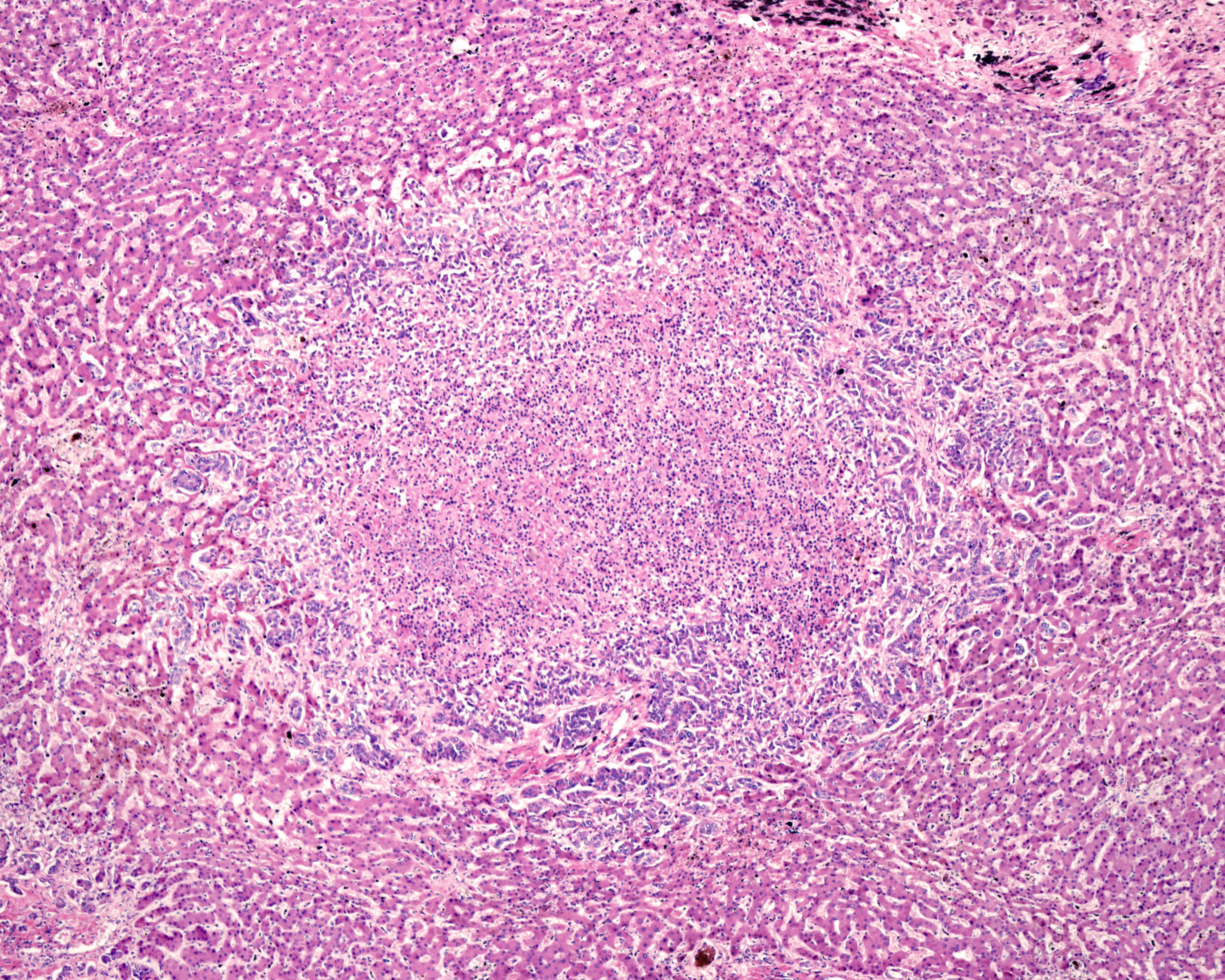
Using single nuclei RNA sequencing, researchers identified the genetic signature of pre-cancerous liver cells known as disease-associated hepatocytes (daHep).
It was then theorised that the more daHep someone has, the higher their chance of developing liver cancer.
Researchers first tested their theory on mice. Then they tested hundreds of patients with liver disease by taking liver biopsies. This confirmed that people who had more daHep cells were more likely to develop cancer.
Prior to this research, the equipment that enabled this discovery did not exist.
“We used a cutting-edge technology to identify the molecular fingerprint of thousands of genes, one cell at a time,” says Rodrigo.
“This technology allowed us to investigate hundreds of thousands of liver cells, which revealed the unique profile of pre-malignant cells.”
How will this change treatment?
Early detection of cancer means patients have more treatment options to try.
However, prevention is always better than treatment, especially when there is no definite cure.
The findings from Rodrigo’s research team gives at-risk people the chance to try and avoid liver cancer.
“If you know you have a high risk, you have the opportunity to alter your lifestyle by following a healthy diet, exercising and reducing your intake of alcohol,” says Rodrigo.
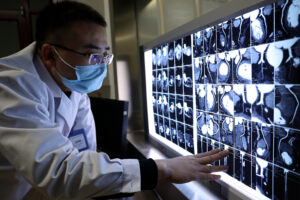
High-risk patients will also have access to intensive monitoring and imaging for early detection of liver cancer.
Next steps
At this stage, the technology is not ready to be used in clinics. The current method requires a liver biopsy, which is invasive and expensive.
“We need to develop a blood test that will test the number of pre-cancerous cells,” says Rodrigo.
This is expected to take around 4 years to develop. However, the team are still in the process of securing funding for this next phase.
“We are excited about the prospect of being able to offer this test to people and help them make the best decisions about their health.”
“We also hope a similar approach can be utilised and applied to the early risk prediction of other cancers.”