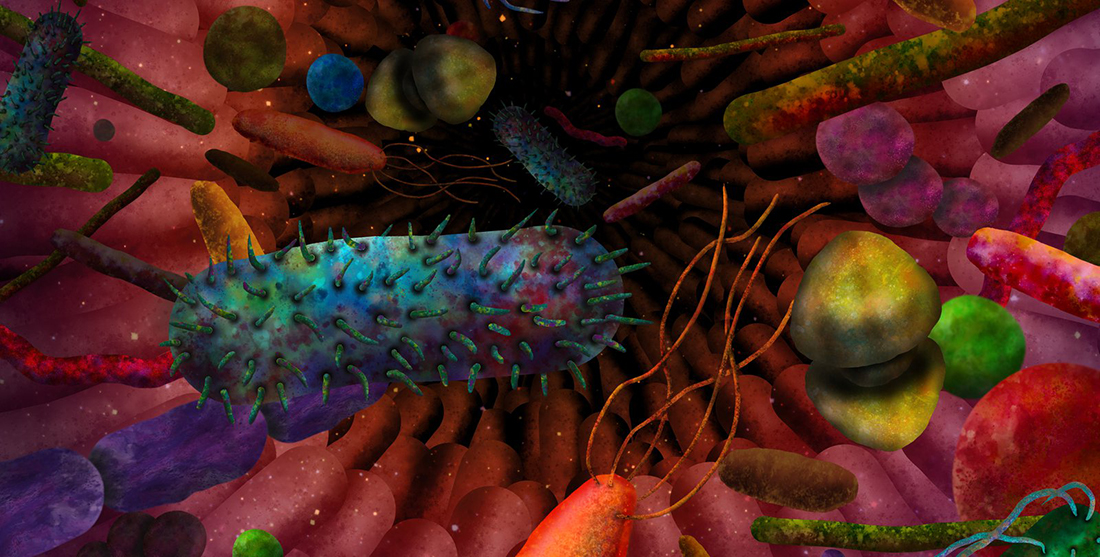
Inside your gut is a collective of bacteria, fungi and viruses known as the gut microbiota.
Amazingly, they start to develop immediately after we’re born. With our mother’s bacteria quickly colonising our body and gut, within weeks, our gastrointestinal tract is loaded with microbes.
This vast community of microorganisms live in our body and are critical for how parts of our bodies operate. In fact, these microorganisms are so important they are as prominent in our body as our own cells.
A gut full
When it comes to our gut, the microbiota is mostly made up of bacteria, although there are also fungi and viruses.
Our gut contains billions of these bacterial cells at any one time, and one of their jobs is to produce essential vitamins our body can’t make, like B1 through to B12, folate, vitamin K and thiamine.
Another important function of these microbes is their influence on the immune system. This is the body’s first line of defence against infections. The immune system also keeps us healthy by eliminating our own cells when they become diseased.
In recent years, the microbes in our gut have been the focus of intense research. What has emerged are strong connections between our health and the presence or absence of specific groups of gut microbes.
Gut microbes and the immune system
Sarkis Mazmanian is Professor of Microbiology at the California Institute of Technology. He’s been studying how gut microbes affect our health for over 15 years.
“Gut microbiota in people varies between individuals,” says Sarkis.
“A new concept has emerged in biomedicine that the balance of different bacterial species in the gut can influence whether the immune system becomes activated or not.”
“This is important, because an overactivated immune system can result in tissue damage and symptoms over time,” he adds.
“[It’s] believed to underlie the cause of many autoimmune, inflammatory and allergic disorders in humans.”
Sarkis believes colonisation with bacteria with anti-inflammatory properties may prevent or even treat many diseases in the future.
Friend or foe?
At the core of an effective immune system is a delicate chemical balance that helps immune cells identify friends from foes. Gut bacteria are important players in this balance. They take the fibre you eat and digest it, turning it into smaller molecules.
One group of these molecules are short-chain fatty acids (SCFAs), a crucial part of our gastrointestinal health. SCFAs can influence a range of cells and functions within the body, leading to changes in the immune function of the gut.
These SCFAs also influence another important immune cell – regulatory T cells.
T cells are the immune system’s informants, telling your body how to respond to invading pathogens or germs.
SCFAs produced by gut bacteria interact with T cells and can influence their behaviour, directing them to attack or spare cells.
Immune system overdrive in type 1 diabetes
Gut microbiota has also been linked to type I diabetes, an autoimmune disease affecting more than 150,000 Australians.
This condition stops the body from producing enough insulin because its own immune system is attacking the pancreatic cells in charge of this task.
In one study, researchers fed mice a number of special diets that were fermented by gut microbes. Dependent on the diet, this led to the production of large amounts of either acetate or butyrate, two common SCFAs produced by gut bacteria. These SCFAs appeared to protect the mice from diabetes.
“What was remarkable about this study was [these] SCFAs protected from diabetes at so many levels,” says Charles Mackay, Professor of Immunology at Monash University.
SCFAs also influence another complex aspect of our biology – our epigenome.
The epigenetic link
Silently working alongside our genome, the epigenome is a vast repertoire of chemical tags placed on DNA molecules that regulate the function of many genes.
Called epigenetic modifications, these chemicals function almost like a coat. When they’re placed on parts of the DNA or associated proteins, they influence their function.
A direct consequence of epigenetic modifications is that genes can be turned on or off, and studies have shown that SCFAs can influence these modifications.
In a 2016 study, researchers found that feeding mice with a Western diet – rich in fat and sugar but poor in fibre – had epigenetic consequences. These mice showed significantly lower levels of Bacteroidetes and a greater amount of Firmicutes (two common type of gut bacteria) compared to mice fed a fibre-rich diet.
“SCFAs, particularly butyrate, can influence the expression of certain genes that have a big impact on biology,” explains Charles.
Other studies have established a link between the gut microbiota, epigenetics and the occurrence of conditions like inflammatory bowel diseases, immune problems and even cancer.
Our unique microbiome
We know it’s important to keep our gut healthy, but one of the biggest challenges is yet to be solved – how do we do it?
“The current state of the art in microbiome research does not provide widely validated ways to improve your microbiome,” says Charles.
“This is largely because more work needs to be done, but also there is likely not going to be a one-size-fits-all intervention.”
Nevertheless, some sure ways to improve the health of your gut and the rest of your body is to eat a healthy diet, rich in fibre and low in fat, sugar and processed foods, as explained by the CSIRO. Also, exercising and sleeping well are a sure way to improve your gut and overall health.