One in four women who have a lump removed from their breast needs more surgery to remove remaining cancer cells.
That’s a pretty scary statistic for patients. And it’s one Professor David Sampson believes could be better.
“One of the main reasons [breast cancer patients need extra surgery] is because all of the tumour is not being identified. Because it can’t all be seen. Because you don’t have the resolution to see it,” David explains.
“So in many instances, resolution – being able to see very small things – is a key part of improving those guidance procedures.”
But what if we had a tool that could help surgeons find even the tiniest traces of cancer during an operation?
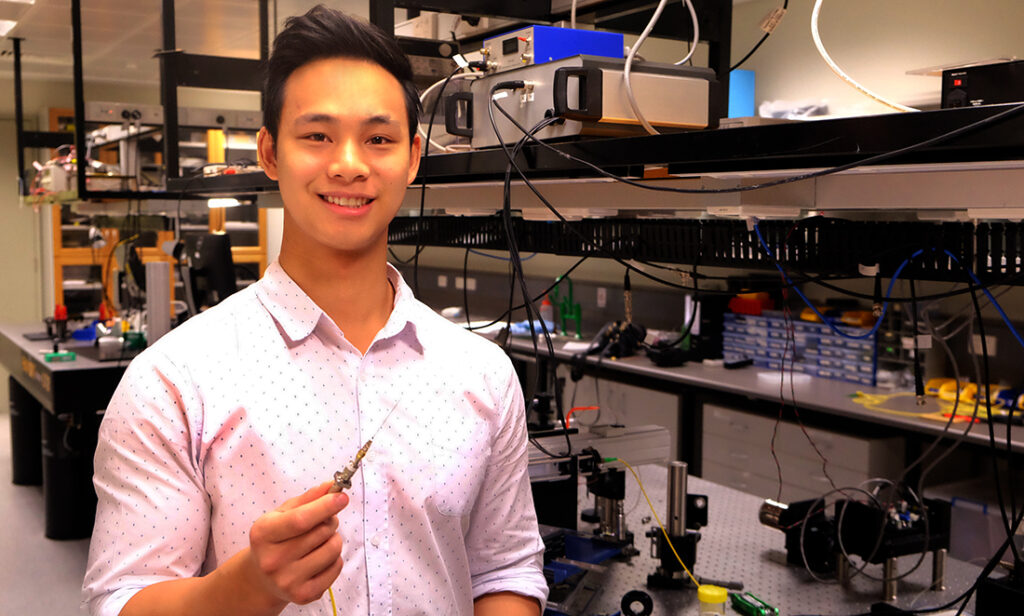
Big things come in small PACKAGES
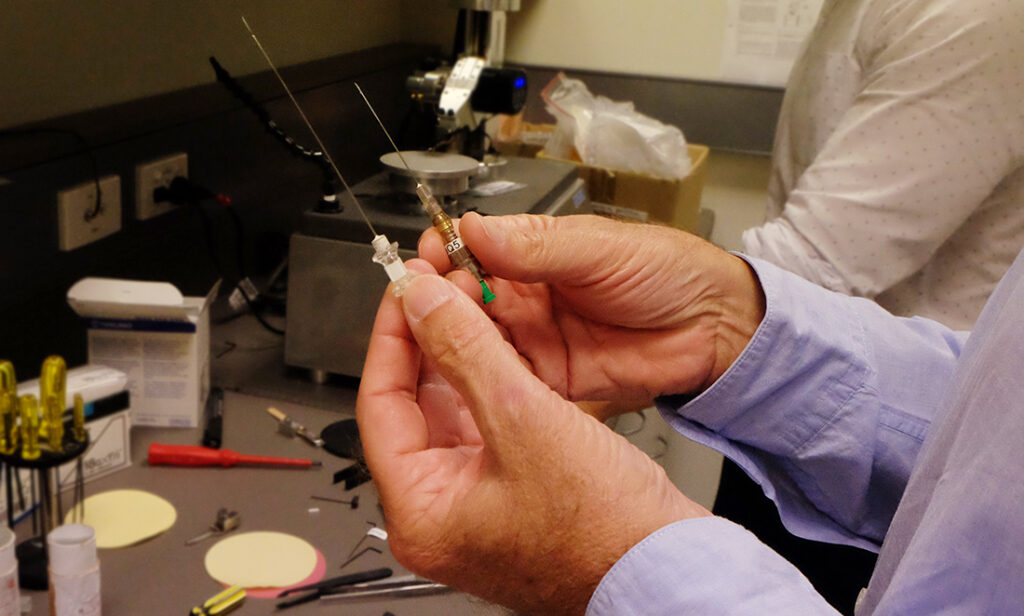
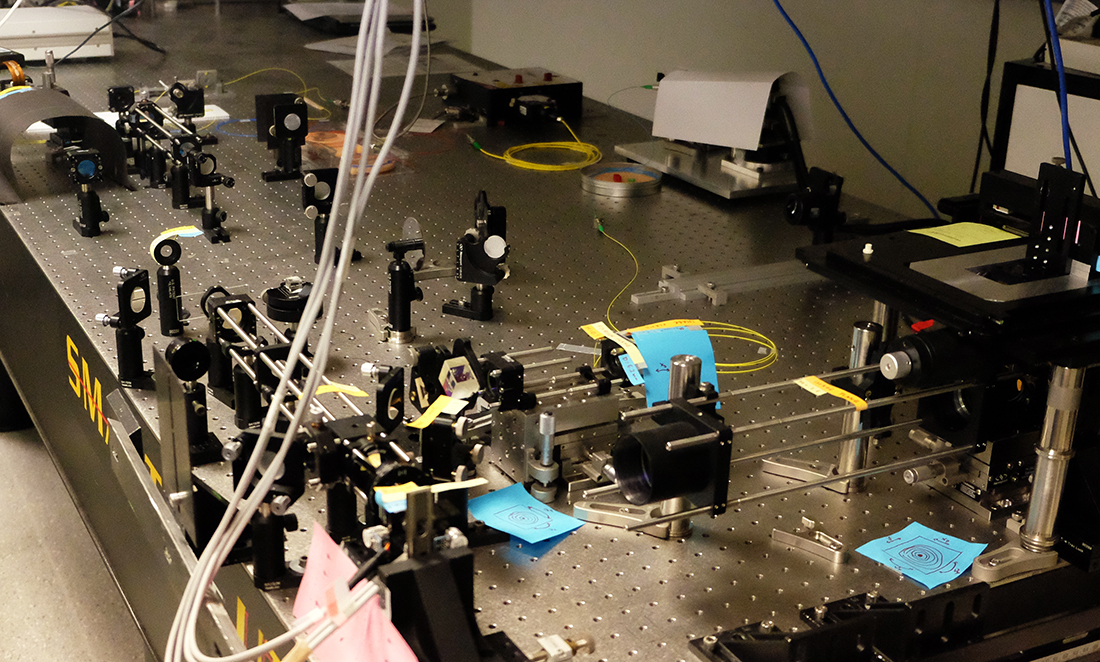
Enter microscope-in-a-needle: The world’s smallest handheld microscope. It’s basically a needle shaft containing optical fibres, which can take images inside tissues at the microscopic level.
“An optical fibre is a very, very small thing. It’s about the thickness of a thick human hair,” he says.
“You can fit quite a few of them down many surgical needles… there’s tonnes of space in there!”
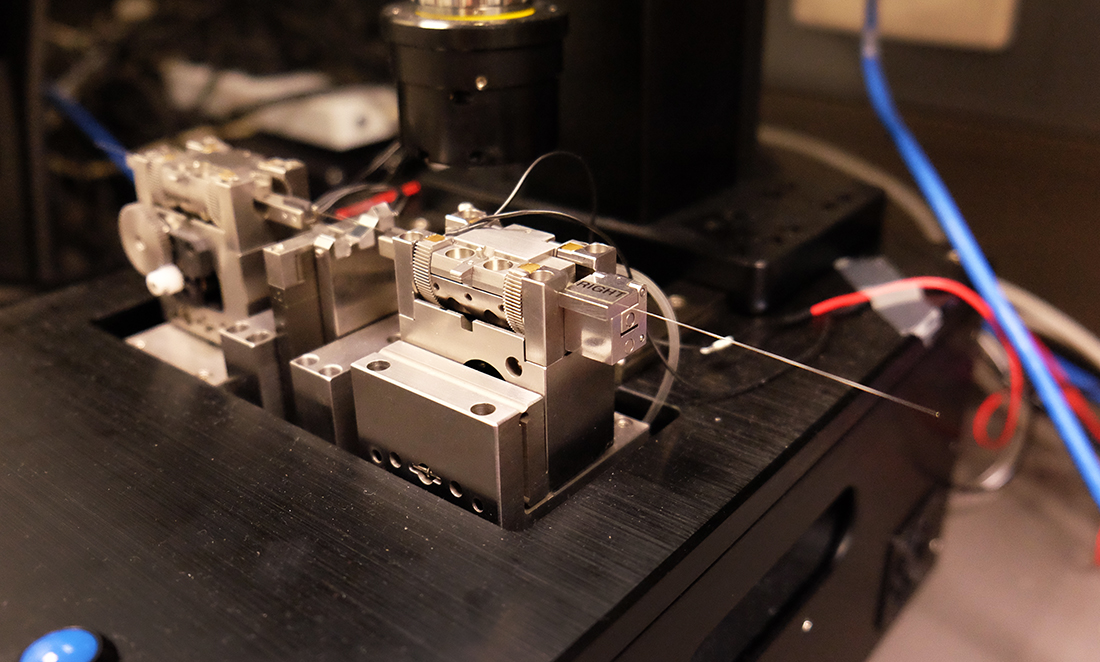
The device uses a technology called Optical Coherence Tomography (OCT). OCT measures where light is bouncing, reflecting and scattering inside the tissue. The needle emits a beam of light. The way that light beam reflects and scatters in the tissue helps build an image of what’s going on inside.
“It essentially measures the time it takes for light to go to a particular location in the tissue and come back. It allows you to pick out just those little beams of light which have gone straight through the tissue, hit something, and come straight back.”
“So we combine that in the needle to provide imaging beyond the end of the needle shaft inside of a tissue.”
Shining a light on cancer
These images have the potential to improve cancer surgeries. They can help the surgeon find trace cancer cells or assist them in identifying the full extent of a tumour.
Another good example is in oral cancer. One of the challenges when removing oral cancers is trying to find the bottom of the tumour. Using microscope-in-a-needle, surgeons could hunt and image until they found the bottom of the tumour. Knowing the exact location means they could remove less tissue during surgery.
“Given that inside your mouth that tissue could be jawbone… could be a piece of your tongue, the consequences are very dramatic in removing the tissue, so the less tissue you can remove the better the surgical outcomes are for the patient.”
But it isn’t just cancer surgery which could be improved by this revolutionary technique. David believes the microscope-in-a-needle could have any number of applications, but they mostly fall into two main categories.
“The main problems [microscope-in-a-needle] will help to attack are based on surgical guidance or biopsy guidance. Either helping the surgeon understand where they’re going in the tissue or actually helping them know they are about to select a sample of tissue that is in exactly the right place.” He explains.
“Those two concepts apply throughout all sorts of different surgery. We initially began doing a lot of work in breast cancer; there is now work going on in brain surgery… there is a lot of potential in prostate surgery – it goes on and on.”
For each potential application of this technology, the needle could be customised to perform the task better. For example, in the treatment of breast cancer, the technology could be more beneficial for surgeons if it could image a larger volume of tissue.
With that in mind, the microscope-in-a-needle could be thought of as the foundation technology for a whole host of new, specialised technologies. This has inspired the research group to re-engineer some of the technologies themselves.
“We’ve got a bunch of things that are actually looking really promising for improving the quality of the images that we get,” he says.
“One of those things is… improving the capacity of the needle to deliver fluids. I think that is a very exciting area… another one is developing the capacity for the needle to feel – to be able to measure stiffness.”
Two Heads are better than one
With so many possible uses to explore, the team can’t do it all themselves. For each application of this technology, there is a lot of work involved with following it through to the end product. Which is why David hopes more people will jump on board with the technology.
“There aren’t enough of us to drive all the possible directions,” he explains.
“What we would love to see is there to be many, many more groups all around the world tackling different applications with the same foundation technology.”
If you’d like to find out more about this exciting tech, check out their website.