If an astronaut spends too much time in space, their body starts to change in some alarming ways.
Their face puffs up and goes red. Their vision starts to go blurry. And the longer they spend in space, the worse it can get.

A year on board the ISS sent blood upwards, causing face puffiness for Scott Kelly and Mikhail Kurnyienko | NASA/Wikicommons
Astronauts orbiting Earth are in free fall and experience microgravity.
This microgravity causes spaceflight-associated neuro-ocular syndrome (SANS).
SANS is a loss of vision that can lead to blindness by deforming the retina.
How does it occur? It’s all about pressure.
EYE DIDN’T SEE THAT COMING
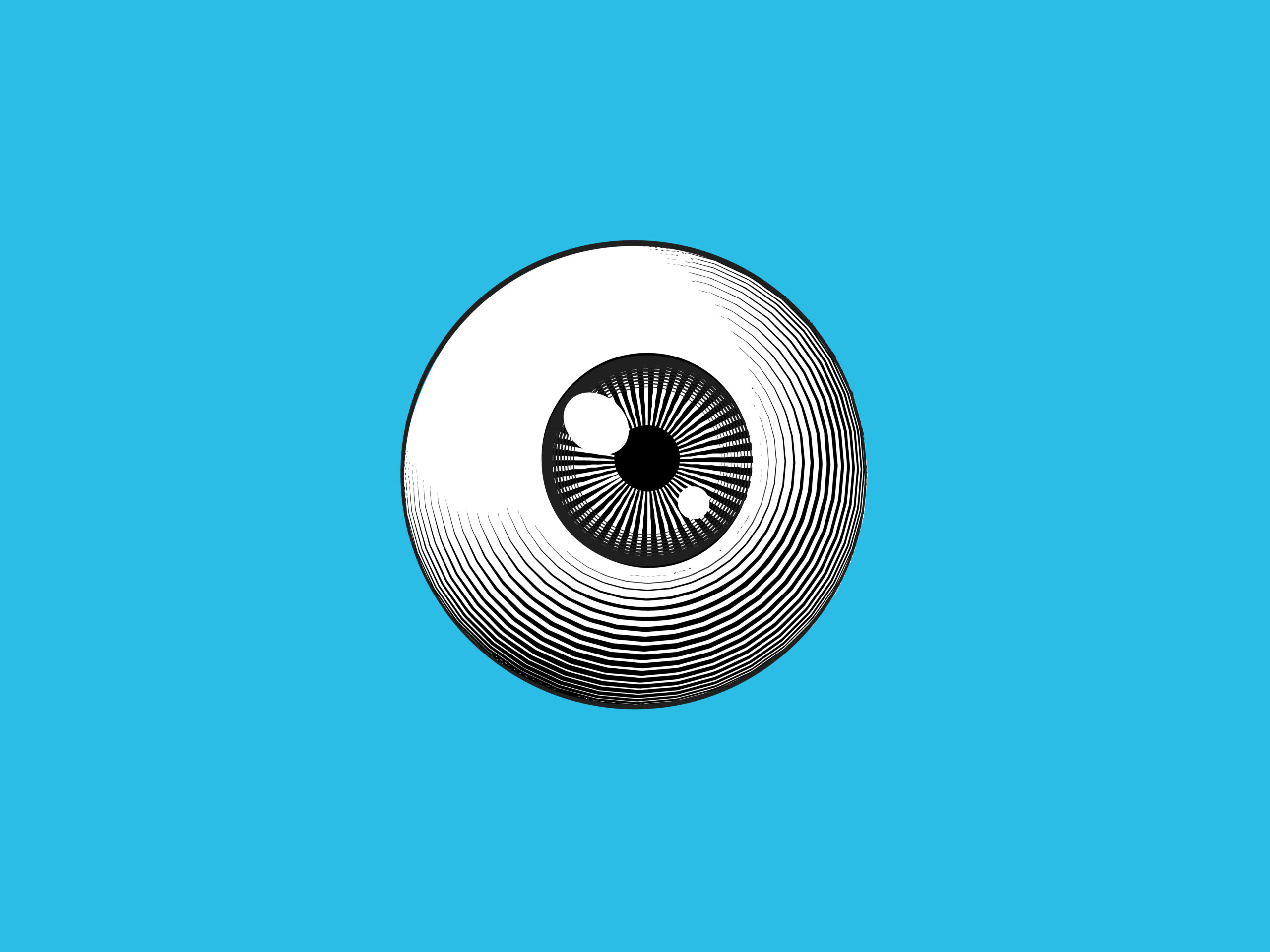
The vitreous humour is the liquid interior of the eye.
It maintains the eye’s shape, protects it from shock and allows light through the eye to enable sight. But pressure from behind the eye can warp its shape.

The retina lines the back of the eye, taking in light and sending signals to the brain | Thomas Crow/Sevier
The body is designed to pump blood up to the brain against gravity.
In microgravity, the resistance against each pump is much less, so fluid pressure in the upper part of your body becomes greater.
“The eyes are in direct contact with the brain,” says Professor Danail Obreschkow, Head of the International Space Centre in WA.
“The fluid in which your brain is suspended, presses against the back of your eyes. This pushes your retina forward a little bit and your vision becomes blurry.”

Images of eye distortions from microgravity – the longer the time spent, the worse the distortion | Danail Obreschkow et al.
UNDER PRESSURE
Danail is an astrophysicist who contributed to the Lions Eye Institute’s new test for SANS.
He’s also a veteran of over 400 parabolic manoeuvres on aircraft. Often called ‘vomit comets’, these are flights with steep descents that allow passengers to experience gravity-free conditions. So he’s spent plenty of time in microgravity.
“If you want to measure the pressure of your brain fluid, you normally drill a small hole in the skull or perform a lumbar puncture in the spine,” says Danail.
“You then put a pressure sensor in the hole.”
It’s as unpleasant as it sounds. But Danail and researchers at the Lions Eye Institute in WA have found an indirect way to measure brain fluid pressure by using imaging techniques for mapping space on the eye.
The group designed a lab in a box that points a camera at the inside of the eye. By filming blood vessels, they can calculate the pressure acting on the eye.
The camera uses light to monitor blood flow within the veins of the retina.
But the eye is a busy place. To let the camera isolate only the important information, Danail introduced a signal processing technique used in astronomy. This technique is most commonly used to clear up images of distant things like stars. But now, thanks to Danail, it’s also being used to take better recordings of the inner eye.
EYES ON THE PRIZE
This research is useful for more than microgravity.
Glaucoma and ocular hypertension both involve pressure damaging the eye.
Of around 300,000 Australians that have glaucoma, half are undiagnosed. Doctors currently diagnose glaucoma by taking a picture of the eye’s optic disc. The optic disc is at the back of the eye where the blood supply and nerve signals flow.
Danail says the team’s invention may help diagnose glaucoma by providing more information than traditional eye exams.
“Brain fluid pressure affects the blood pulsations in your retina,” says Danail.
By taking a video of the blood vessels pumping, the team can see if brain fluid pressure is distorting the eye.
“We observe the pulsations of the small blood vessels and deduce the pressure. Then we can say if that’s likely to distort the eye.”
THE EYES HAVE IT
This cutting-edge device could improve how we diagnose some eye problems in space and on Earth. But it weighs 100kg, so you won’t find it at your local optometrist’s office just yet.
According to Danail, the device is “a whole laboratory full of stuff inside.”
“There is an optical bench, there is a computer on it and there are cables for the camera. But the vast majority of those things can be miniaturised with absolutely no problem.”
So what’s the next step to make this tech more widely available?
According to Danail, if the device’s functions can be put on a microchip, it could be turned into a hand-held device.
If the Lions Eye Institute’s ‘lab in a box’ can be made smaller, it could diagnose SANS for the next generation of astronauts and earthbound patients.
Wouldn’t that be a sight to see?