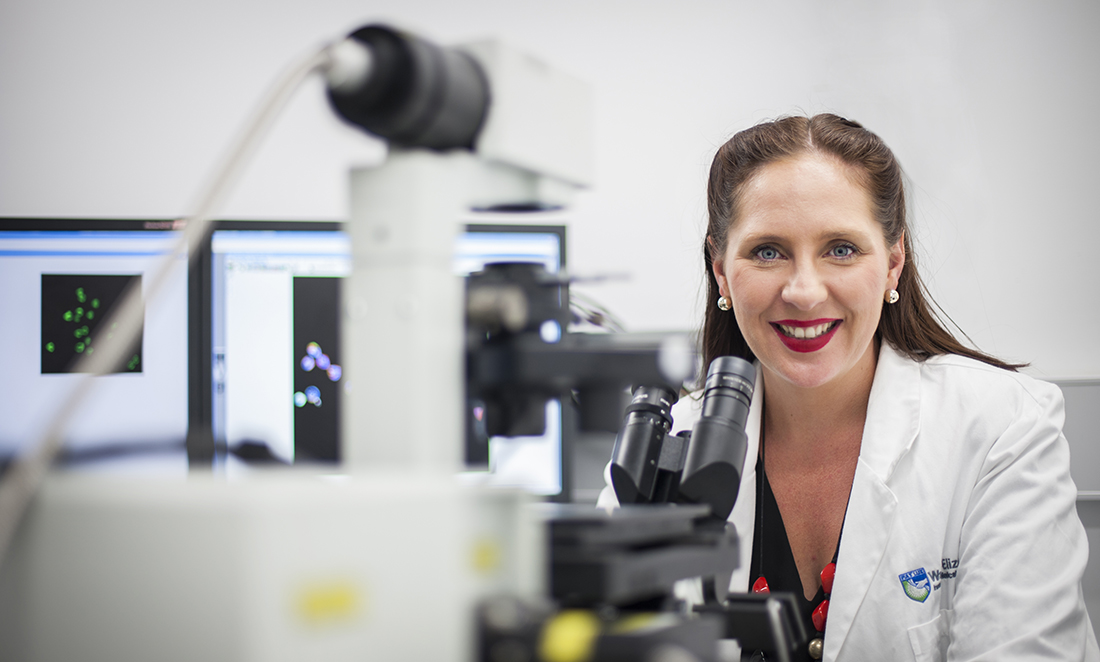
Since 2016, Misty has led a lab at the Walter and Eliza Hall Institute of Medical Research.
From a young age, Misty was fascinated with how the body works. This fascination inspired her to complete a Bachelor of Science, where she discovered a passion for learning about white blood cells.
Cell snipers
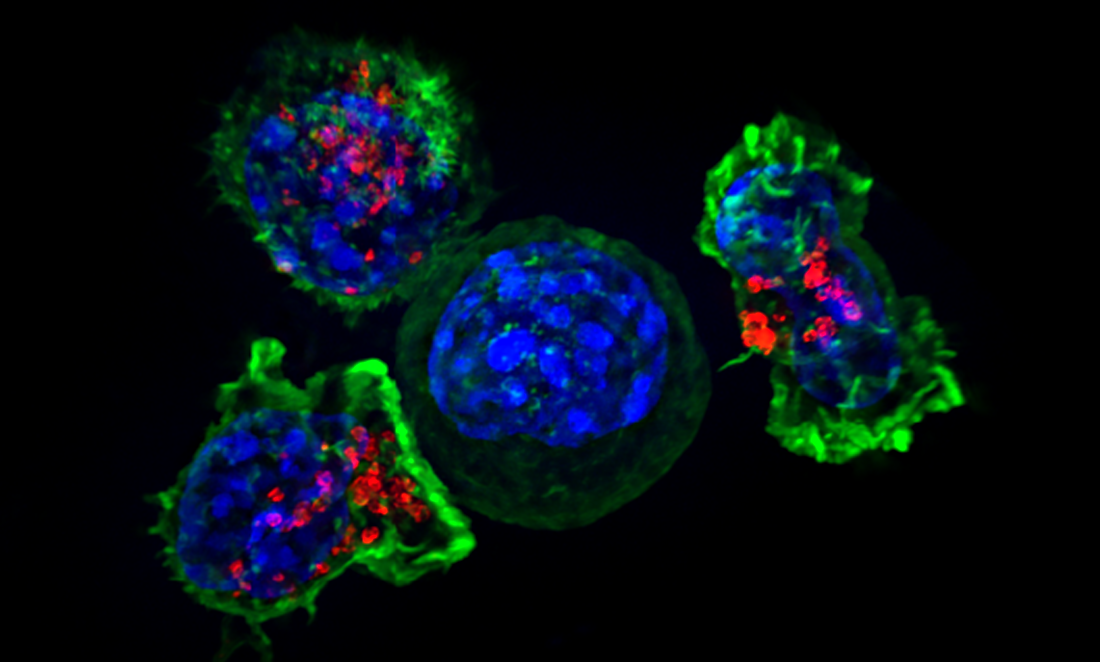
Killer lymphocytes are a subset of white blood cells that protect our bodies from viruses and cancer.
Misty describes them as an army being sent off to destroy invaders in the cell.
“They’re zooming around in the blood and lymph system, trying to keep us healthy.”
“Most of the time, they do a really good job, but when they don’t, we can develop cancer,” she says.
During her PhD, Misty looked at how the killer lymphocytes arm themselves.
“War is a really good analogy—soldiers play different roles,” she says.
There is a specialised subset called killer T cells that kill cancerous and virus-infected cells.
“I looked at how they choose their weapons.”
Misty says killer T cells destroy their targets by throwing toxic grenades at the cancer cell.
“There are many different kinds of weapons, and during my PhD, I examined what regulates the acquisition of T cell killing machinery.”
“The more we understand how T cells kill, the easier it is for us to manipulate the system.”
Her fascination with these cells led her to cancer immunology-immunotherapy work.
An immunology arms race
“There have been monumental leaps in how we can manipulate our immune system and rearm it against invaders,” Misty says.
“We are now engineering blood cells to arm the immune system against the patient’s own tumour.”
In terms of cancer therapy, treatments for cancer have advanced from surgery to radiation, X-rays and chemotherapy.
“We’ve come such a long way in the last decades in how to manipulate our immune system,” she says.
Misty says immunotherapy will provide a whole new fourth pillar of therapy—harnessing the power of the immune system.
“We are now engineering blood cells to arm the immune system against the patient’s own tumour.”

Misty says scientists and doctors can take a patient’s blood and genetically engineer their white blood cells to redirect them against their own tumour.
“This occurs by giving the white blood cells the receptor they need—the key to fit the lock—of the tumour cells.”
Misty’s projects use a variety of cutting-edge techniques to answer complex scientific problems. She is known widely for her use of live cell microscopy, which is like taking a digital picture of the cells to examine their behaviour.
Her research is aiming to understand how killer lymphocytes acquire the ability to kill and detach from cancer cells.
“We want to learn about the interplay between lymphocytes and other immune cells and the subsequent consequences for the immune system,” she says.

In recognition of her research excellence, Misty has won numerous awards and funding support, including a prestigious University of Cambridge College Fellowship, and she was one of the 2016 Westpac/AFR Top 100 Women of Influence.
She was most recently awarded the CSIRO Indigenous STEM Professional Career Achievement Award.
Into the future, Misty’s primary focus is her lab and discovering innovations to bring new cancer immunotherapy to clinical trials.
The biggest success for this type of therapy, Misty says, has been for blood cancers, and there has only been moderate success in solid cancers, as they have additional challenges.
“My lab is examining how we might apply this therapy to the brain,” she says.