The COVID-19 vaccine was unique. It used mRNA, which teaches the human body to make proteins to fight off the disease.
Now, scientists have found that mRNA vaccine technologies could be used to prevent or help control HIV.
BACK TO BASICS
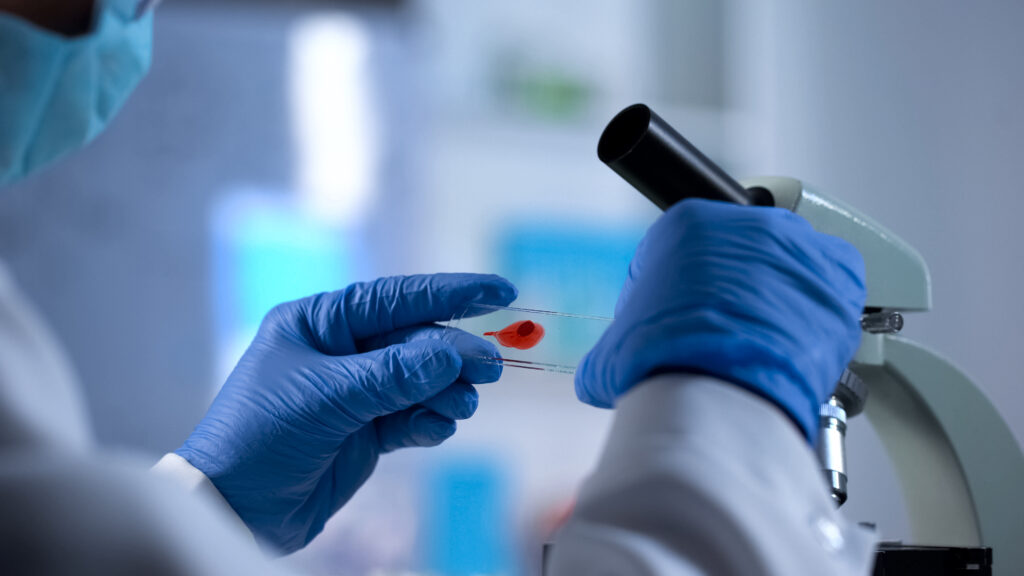
Traditional HIV vaccines target a protein on the surface of the virus. It appears spiky and is the part of the virus that latches on and enters human cells.
Block this, and the virus can’t get in.
Early vaccine attempts explored the use of dead or weakened versions of the virus. However, safety concerns encouraged scientists to move towards simulating parts of the virus instead.
One approach focused on synthetic free-floating versions of the protein to trigger an immune response. Unfortunately, this method doesn’t always work.
If the protein is free floating, the immune system may target the wrong part of the protein that is inaccessible when attached to a membrane like the real virus.

Credit: MargJohnsonVA/Getty Images
A NEW WAY FORWARD
To avoid this problem, researchers are looking to mRNA vaccines.
These vaccines act like recipes. Cells read the vaccine instructions and create specific viral proteins to trigger an immune response against the virus.
Following one of the vaccine recipes, cells can create membrane-bound proteins that simulate the HIV virus. This ensures a more efficient immune response.
This method better mimics the effect a real HIV infection has on the human body.
As mRNA can be designed and produced quickly, it enables a flexible and fast way to test different versions of a vaccine to find the best fit.
Credit: Mortortion/Getty Images
A GAME-CHANGER IN GLOBAL HIV PREVENTION
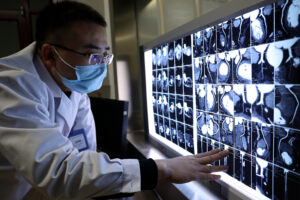
Initial studies found the mRNA vaccine effective in rabbits and macaques. Now, researchers are doing a clinical trial in humans.
The human trials investigated different types of mRNA HIV vaccines. One of the vaccines looks particularly hopeful, with 80% of people creating an effective immune response to neutralise HIV.
While there is still a long way to go to study larger and more diverse groups, the vaccine’s potential is undeniable.
For people at higher risk of HIV, a vaccine could offer affordable protection for those in low-socioeconomic areas and alleviate some of the fear and judgement towards marginalised groups such as the LGBTQIA+ community.
It’s a significant advance for vaccine technology and offers hope for effective and affordable prevention of HIV in the future.